Pain is a common human sensation that can vary from a small annoyance to a crippling illness that interferes with daily functioning. Historically, a lot of pharmaceuticals have been used to treat pain, especially nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids. Although these treatments have the potential to be beneficial, they frequently have serious adverse effects and have a dependency risk. The necessity for more creative and all-encompassing methods of treating pain has been acknowledged by the medical profession more and more in recent years. This article examines a number of cutting-edge techniques that are revolutionizing pain treatment and providing millions of patients with hope and a higher standard of living.
The Opioid Epidemic and Alternatives Seeking
The hunt for non-opioid painkillers has been greatly accelerated by the opioid crisis. The overprescription of opioids has resulted in a high rate of addiction and death, which has forced medical professionals to reevaluate their approaches to treating pain. The urgency of finding safer, non-addictive pain relief alternatives has been highlighted by this problem, which has also sparked research into a range of novel medicines.
Nonpharmacological Approaches
The focus on non-pharmacological therapies is one of the most exciting developments in contemporary pain management. These approaches try to treat pain without using drugs exclusively, which lowers the possibility of addiction and other negative side effects.
1. Rehabilitation with physical therapy
The foundation of non-pharmacological pain management is physical therapy. It entails physical activities and therapies intended to lessen pain while enhancing strength, function, and mobility. Physical therapists collaborate with patients to develop customized treatment regimens that target the unique sources of their pain. Pain relief and quality of life can be greatly enhanced by methods like manual therapy, stretching, strengthening exercises, and the use of heat, cold, and ultrasound modalities.
2. CBT, or cognitive behavioral therapy
A psychological strategy called cognitive behavioral therapy (CBT) aids patients in comprehending the connection between their feelings, ideas, and actions. The goal of cognitive behavioral therapy (CBT) for pain management is to alter unfavorable thought processes that may worsen pain perception. CBT helps patients enhance their general well-being and lessen the emotional discomfort brought on by chronic pain by teaching them coping mechanisms and problem-solving techniques.
3. Body-Mind Methods
Pain management therapies that focus on the mind-body, such tai chi, yoga, and mindfulness meditation, are becoming more and more popular. By highlighting the relationship between the mind and body, these techniques help people relax and cope with stress, both of which can help people feel less pain. For instance, mindfulness meditation can lessen the intensity of pain and increase emotional resilience by encouraging patients to accept their experience in the present moment and without passing judgment.
4. The use of acupuncture
In order to regulate energy flow and encourage healing, acupuncture, an ancient Chinese medical procedure, involves inserting tiny needles into particular body locations. Studies have demonstrated the efficacy of acupuncture in treating a variety of pain conditions, such as migraines, osteoarthritis, and back pain. It is thought to function by decreasing inflammation and promoting the body’s natural painkillers, such as endorphins.
Developments in Pain Management Technology
The field of pain management has also undergone a technological revolution, with new tools and approaches that both improve and introduce established practices.
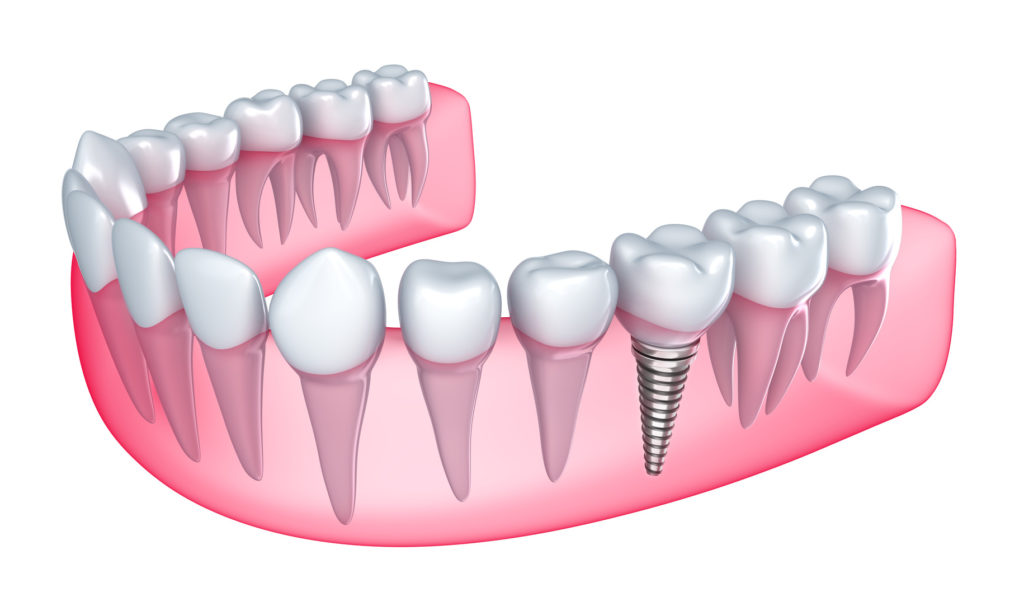
1. The function of neuromodulation
The modification of nerve activity by the focused application of pharmacological or electrical stimuli is known as neuromodulation. Spinal cord stimulation (SCS) is one of the most well-known types of neuromodulation. It entails implanting a gadget that stimulates the spinal cord with electrical impulses in order to block pain signals before they reach the brain. Deep brain stimulation and peripheral nerve stimulation are two more types. Chronic back pain, neuropathy, and even excruciating headaches can all benefit greatly from these treatments.
2. Therapy Using Virtual Reality (VR)
A newer form of treatment called virtual reality (VR) employs immersive virtual surroundings to help patients feel less pain and divert their attention from it. VR therapy can be especially helpful in instances where there is acute discomfort, including during medical operations or the recovery period following surgery. It functions by involving the brain in a highly interactive experience that can cause the focus to change from pain to relaxation and overall well-being.
3. Technology Wearables
Advanced wearable technology is being used to monitor and control pain. These gadgets monitor sleep habits, physical activity levels, and other variables that affect pain thresholds. Certain wearables provide electrical impulses to lessen pain, such as transcutaneous electrical nerve stimulation (TENS) units. Others employ biofeedback to assist patients in comprehending their physiological reactions and creating more effective pain-management plans.
Pharmaceutical Advancements
While non-pharmacological treatments have emerged in response to the need for non-addictive, efficient pain alleviation, pharmaceutical advancements continue to play a crucial role in pain management.
1. Alternative Medicines
New families of non-opioid drugs that address pain without having the same addictive potential as opioids are being developed by researchers. For example, chemicals called cannabinoids, which are obtained from the cannabis plant, have demonstrated potential in the treatment of chronic pain. Many drugs are currently approved for use in medicine, including tetrahydrocannabinol (THC) and cannabidiol (CBD), which are being investigated for their analgesic qualities.
2. Biologicals
Biologic medications represent a potentially viable approach to pain relief as they are sourced from living creatures. These medications specifically target immune system components linked to pain and inflammation. For instance, the potential of monoclonal antibodies that block nerve growth factor (NGF) to alleviate persistent pain problems including osteoarthritis and persistent lower back pain is being studied.
3. Customized Health Care
Personalized pain management is becoming possible thanks to developments in biotechnology and genomics. Healthcare professionals may better adapt therapies to the unique needs of each patient by knowing their genetic composition, which maximizes efficacy and minimizes negative effects. More potent pain management techniques may result from this method, especially for individuals who have not reacted well to traditional therapies.
Complementary Pain Management
Integrative pain management treats the physical, emotional, and psychological components of pain by combining traditional medical care with complementary and alternative therapies. This all-encompassing approach acknowledges that pain is a complicated experience impacted by a range of causes and that a diverse approach is necessary for effective therapy.
1. Pain clinics with many specialties
In order to create comprehensive pain management programs, multidisciplinary pain clinics bring together medical practitioners from a variety of disciplines, such as psychology, physical therapy, medicine, and alternative therapies. These clinics provide a team-based approach that takes into account each patient’s particular needs and makes sure that every facet of their pain is taken into account.
2. Instruction for Patients and Self-Management
Integrative pain management’s primary goal is to provide patients with the information and abilities they need to control their own pain. Patient education programs educate patients on the types of pain they experience, the treatments that are available, and how to take care of themselves. Self-management strategies can help patients take charge of their pain and enhance their quality of life. These strategies include timing activities, relaxation exercises, and making healthy lifestyle choices.
Pain Management’s Future Directions
The combination of many techniques and ongoing innovation are key components of the future of pain management. More efficient and individualized pain management techniques will result from ongoing research into the mechanisms behind pain, the creation of novel therapies, and the improvement of current techniques.
1. Progress in the Study of Pain
It is essential to comprehend the many mechanisms behind pain in order to create novel remedies. Studies in the domains of neuroscience, immunology, and genetics are providing insights into the mechanisms behind pain and pinpointing possible avenues for remediation. This information will guide the creation of cutting-edge pain management treatments that are less likely to have negative side effects.
2. Comprehensive and patient-focused methods
It’s likely that the trend toward patient-centered, holistic care will continue, with a focus on treating the full individual rather than just their pain symptoms. This method entails taking into account the social, emotional, and physical components of pain and creating individualized treatment programs that take into account each of these factors.
3. Cooperation and Multidisciplinary Medical Care
Progress in pain management will require cooperation across many medical specialties. The best complementary, psychological, and medical therapies can be combined in a holistic strategy by interdisciplinary care teams. Patients are guaranteed to receive the most comprehensive and successful care possible because to this collaborative approach.
In summary
Reimagining pain management entails eschewing conventional techniques and adopting a broad spectrum of cutting-edge strategies. The field of pain treatment has a lot of potential for the future, from non-pharmacological therapies and technology breakthroughs to pharmaceutical breakthroughs and integrative care. Millions of people who suffer from pain can live better lives if healthcare providers take a more comprehensive and patient-centered approach to providing more long-lasting and effective pain management solutions. The potential for pain management will only increase as science and technology develop, giving those in need hope and healing.